Abstract
Introduction
Primary immune thrombocytopenia (ITP) is caused by the destruction of platelets (PLT) and megakaryocytes by autoantibodies, cellular cytotoxicity, or/and impairment in PLT production. Thrombopoietin-receptor agonists (TPO-RA) are a commonly used therapy in ITP that activate JAK/STAT pathways, stimulating megakaryocyte growth and PLT production. TPO-RAs, which include eltrombopag (EPAG), are effective in restoring PLT count in 70-80% of cases with chronic ITP. Recently, it has been observed that PLTs have an immunoregulatory role and their binding to lymphocytes and monocytes can modulate leukocyte inflammatory profile. Our aim was to determine the percentage of lymphocytes with bound PLTs before and after EPAG treatment, analyzing factors associated with this binding and with response.
Methods
For this purpose, peripheral whole blood was collected from 43 ITP patients relapsed/refractory to corticosteroids (at baseline and 2, 4, 12, and 18 w after the initiation of EPAG) and 15 healthy donors (HD). The percentage of T CD4+, T CD8+, and B lymphocytes with bound PLTs (CD41a+) were analyzed by flow cytometry and plasma levels of cytokines (IFN-γ, TNF-α, IL-10 and IL-17) by ELISA.
Results
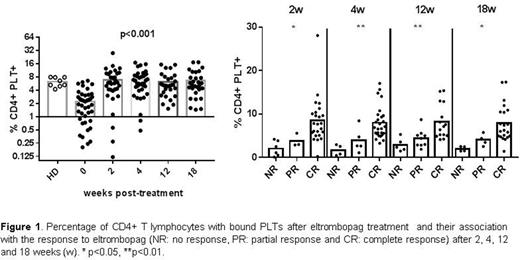
In comparison with HD, the absolute number of PLTs was lower and the percentage of free activated PLTs was higher in ITP patients at baseline. Additionally, the percentage of T and B lymphocytes with bound PLTs in ITP patients was lower than in HD. After 2w of EPAG treatment, the percentages of T and B lymphocytes with bound PLTs were normalized and IFN-g levels were reduced. However, no significant changes were observed in the percentage of free-activated PLTs and in the percentage of T and B lymphocytes with bound activated PLTs. The percentages of T and B lymphocytes with bound PLTs were higher in ITP patients that reached complete response (>100 x 109 PLT/L without bleeding) compared with partial response (30-100 x 109 PLT/L) and non-response (<30x 109 PLT/L) patients in each time point of the study after EPAG treatment (Figure 1).
Conclusions
Our results suggest that the increase of PLTs after EPAG treatment is not only mediated through the platelet production stimulation, but also through the increase of PLT binding to lymphocytes which may influence the inflammatory profile of ITP patients. This newly mechanism of action could explain the persistent response of ITP patients after EPAG treatment.
Disclosures
Novelli:Mundipharma: Consultancy; Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal